How Free Mental Health Drugs are being sold in Volta Region at the Ho Municipal Hospital
DAILY Analyst can report that both the Mental Health Unit (MHU) and the Ho Municipal Hospital in the Volta Region have commissioned investigations into the sale of mental health drugs that are supposed to be administered and offered to patients for free.
This was uncovered following a painstaking investigation conducted by DAILY Analyst. Our findings revealed how government supplied psychotropic drugs including olanzepine, risperidone, amitriptyline, carbarmazepine and flouxetine were being sold to poor patients at very high prices for personal gains.
- Advertisement -
It emerged from our findings that the practice which was being recorded at the Ho Municipal Hospital was widespread involving unit heads taking advantage of the situation and cashing in on poor patients.
- Advertisement -
For instance, the paper found out that some of staff members of Ho MHU and Ho Municipal Hospital make a whopping sum of GH¢1,500 on a daily basis from the sale of these drugs to unsuspecting patients.
And the sale of these drugs ranged from GH¢ 40.00 and GH¢60.00, the paper was reliably informed. Though the hospital was tight-lipped on the matter, information filtering in indicated that the hospital administration had already opened an internal investigation into the matter.
Corroborating our story, a Deputy Director at the Volta Region’s Health Directorate, Mr Robert Adatsi, in an interview with DAILY Analyst, said the canker was a nationwide problem, which had been compounded by the lack of regular supply and shortages of mental drugs to the mental health facilities.
Read More:
“In fact, there are issues. If you dwell on the Volta Region alone, that is just a drop in the ocean—it is a national issue,” he said.
“We have proposed that mental health treatment be rolled onto the National Health Insurance Scheme but that has not been done,” he said.
“So what we are seeing now is as a result of how the system was functioning. I strongly believe that if mental health treatment is rolled onto the National Health Insurance Scheme, there will be adequate management of medicines, and there wouldn’t be any gap for middlemen and women, even if they should, they would have gone through proper procurement processes,” he submitted.
- Advertisement -
According to Mr Adatsi, some private individuals also penetrate the system through mental health practitioners who act as middlemen and women. These so-called middlemen and women, he said, take advantage of the gaps in the system to advertise their medicines, making the illegal practice to linger on.
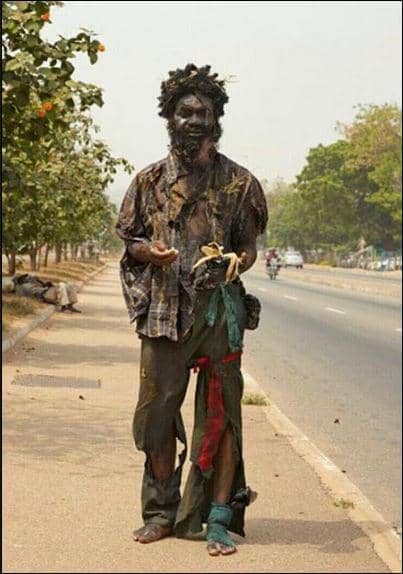
He also added that these systemic gaps compel mental health practitioners to fall on those middlemen and women at a very high price. It would be recalled that in 2010, some damning secrets were brought out by ace investigative journalist, Anas Aremeyaw Anas, with his ‘MadHouse’ documentary on the Accra Psychiatric hospital.
The documentary revealed how mental patients were stigmatised and their free drugs sold to them despite the difficult situations they were faced with.
There are three mental hospitals in Ghana with a total of 1,322 beds (5.5 beds per 100,000 population).
Two of which are located in the national capital—Accra—and the other located in the Central Region of Ghana which is also in the south of Ghana. The government’s policy on mental health care has always been and remains to provide psychiatric treatment, including admissions and all medications, for free.
In the face of a very small budget, the range and quantities of medications provided is often grossly inadequate. This was according to findings. There is a turnaround time of around two years in the public procurement cycle, and in practice, most medications are only accessible in the specialist public psychiatric facilities, which often procure them from private pharmacies (or through private donations).
According to reports, in less urban areas, most pharmacies do not find it cost-effective to stock psychopharmacological agents beyond the most basic (and usually inappropriately used) benzodiazepines.
Reports again has it that the overall result is long periods of shortages of medication, which mostly lead to relapse of illness, and in the case of epilepsy, dangerous recurrence of seizures.
Costs are generally affordable for the few drugs made available through the state system, but most patients are unable to afford medication, even if they can be obtained from private sources.
It was advised that the real challenge is making an appropriate range of medications easily available at all times to patients within the policy of free care. It is against the above that some concerned patients and stakeholders are calling for a broader investigation into this rather unfortunate development so that the perpetrators will be brought to book.
Source: Freeman Koryekpor Awlesu II
DAILY Analyst
- Advertisement -